Fibrillin-1
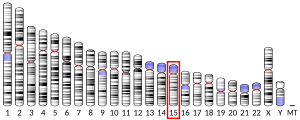
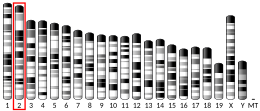
Fibrillin-1 is a protein that in humans is encoded by the FBN1 gene, located on chromosome 15.[5][6] It is a large, extracellular matrix glycoprotein that serves as a structural component of 10–12 nm calcium-binding microfibrils. These microfibrils provide force bearing structural support in elastic and nonelastic connective tissue throughout the body. Mutations altering the protein can result in a variety of phenotypic effects differing widely in their severity, including fetal death, developmental problems, Marfan syndrome or in some cases Weill-Marchesani syndrome.
Gene
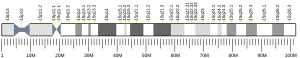
[edit]FBN1 is a 230-kb gene with 65 coding exons that encode a 2,871-amino-acid long proprotein called profibrillin which is proteolytically cleaved near its C-terminus by the enzyme furin convertase to give fibrillin-1, a member of the fibrillin family, and the 140-amino-acid long protein hormone asprosin.[7][8]
Structure
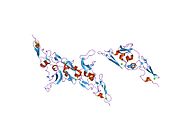
[edit]The sequence of fibrillin-1 includes 47 six-cysteine EGF-like domains, 7 eight-cysteine domains homologous with latent TGF-beta binding protein, and a proline-rich region.[9]
Function
[edit]Fetal cardiovascular development
[edit]The FBN-1 gene is involved in a variety of embryonic developmental programs. The microfibrils that are made from fibrillin-1 contribute to both elastic and non-elastic structures. The formation of the elastic fibers in the heart valves and the aorta require the involvement of both FBN-1 and FBN-2.[10] It has been shown that both FBN-1 and FBN-2, along with the other components of elastic fibers, are expressed in the embryonic semilunar valves as early as 4 weeks of gestation.[11] These molecules interact to form the elastic fibers in the ventricularis layer of the semilunar valves. Fibrillin-1 and fibrillin-2 are also crucial for the development of elastic fibers in the aorta. While expression of fibrillin-2 decreases significantly after fetal development, the expression of fibrillin-1 continues into adulthood. This supports the idea that fibrilin-2 dictates the development of early elastic fibers, while fibrillin-1 provides the structural support of mature elastic fibers.[11]
When mutations in the FBN-1 or FBN-2 genes occur, significant deformations can result from the damage to the extracellular matrix. Marfan syndrome is a congenital disease that arises from a mutation in the FBN-1 gene. This leads to the malformation and subsequent weakening of the microfibrils in the patient’s body, including the structures of the cardiovascular system. The weakened elastic fibers will result in an impaired durability and distensibility in the heart valves and aorta. This provides the explanation for the aortic aneurysms and prolapsed valves that are commonly associated with Marfan syndrome.[12]
Clinical significance
[edit]Mutations in the FBN1 gene are associated with Marfan syndrome and its variant Marfanoid–progeroid–lipodystrophy syndrome, autosomal dominant Weill–Marchesani syndrome, isolated ectopia lentis, MASS phenotype, and Shprintzen–Goldberg syndrome.[13][14]
Mutations in FBN1 and FBN2 are associated with adolescent idiopathic scoliosis.[15]
Clinical symptoms of MFS such as aortic root dilation, pulmonary emphysema, atrioventricular valve changes and skeletal muscle myopathy are induced by altered TGF-β activation and signalling.[16] Aortic specific symptoms are closely related to excessive TGF-β signalling in the aortic root wall.[16] TGF-β antagonism via systemic administration of TGF-β neutralising antibody (NAb) averted the development of aortic pathologies associated with MDS, more specifically changes in the aortic wall and progressive aortic dilation.[16] Antagonism of TGF-β also further reduced MFS symptoms where it helped muscle regeneration, architecture and strength, pulmonary alveolar septation and mitral valve morphology.[16]
Mutations
[edit]FBN1 is a gene approximately 200kb and is made up of a large coding sequence divided into 65 exons located on chromosome 15. This gene encodes for Fibrillin-1 protein.[17] Fibrillin-1 is a large cysteine rich-glycoprotein approximately 350 kDa mainly composed of tandemly repeating domains of epidermal growth factor (EGF)-like modules. These domains are homologous to calcium binding epidermal growth factor module (cbEGF-like motifs) and of distinct 8-cysteine modules to make up elastic and non-elastic tissue.[18][19] These elastic and non-elastic tissues are microfibrillar bundles, heteropolymers of both Fibrillin-1 and fibrillin-2.[20] Elastogenesis is a biological process where microfibrils and elastic fibres are self-assembled via organised deposition by several macromolecules.[21] Polymerised fibrillins can be characterised by their ‘beads-on-a-string’ microfibril structure; giving rise to a microfibril lattice via lateral communication of the individual polymers and structural components.[21]
Fibrillin-1 mutations are the main mutated protein causing MFS. This mutation usually interferes with the assembly of microfibrils resulting in a dominant-negative mechanism [18][22]
Mutations can include:
- Missense mutations caused by single base substitutions such as cysteine or those associated with calcium binding in Fibrillin-1.[17]
- Premature terminations caused by nonsense mutations or frameshifts.[17]
- Mutations within the exonic splice site allowing for insertions or deletions due to creations of cryptic splice sites.[17]
- Intronic splice site base changes leading to alternative splicing and in-frame exon skipping or deletion.[17]
The combination of the four types of mutations results in Fibrillin-1 being expressed incorrectly. There is no correlation between phenotype and genotype at a molecular level [17]
The mutations of the FBN-1 gene at six chromosomal loci, TAAD1 at 5q13-14, FAA1 at 11q23-24, TAAD2 at 3p24-25, TAAD3 at 15q24-26, TAAD4 at 10q23-24 and MYH11 at 16p12-13 are known to be triggers of MFS.[23] These loci tend to have genes that are involved in vascular function.[23] The MYH11 gene is responsible for the smooth muscle myosin heavy chain and ACTA2 at TAAD4 loci encodes for smooth muscle alpha-actin.[23]
A nonsynonymous amino acid change affecting conserved cysteine of the CaB-EGF-like domain encoded by exon 13 of the FBN1 gene can cause MFS to develop.[21] Higher frequency and severity of MFS occurs when there are incorrect substitutions at the C1–C2 or C3–C4 disulphide bonds, therefore, correct cysteine localisation and disulphide bonding at these loci are critical to structural integrity.[21] Mutations in the FBN1 gene resulting in incorrect bonding at the C5–C6 disulphide bond generally results in MFS of lesser severity.[21] Concentrated mutations of the CaB-EGF domain along the FBN1 polypeptide affects MFS severity phenotype.[21] Localised substitution mutations of the cysteine substitution at C538P on exon 13, C570R on exon 14 or C587Y on exon 15 result in MFS symptoms related to the eyes, specifically ectopia lentis.[21] Microfibrils themselves can support the hemodynamic load in the circulatory systems of invertebrates and lesser vertebrates.[21] Elastin and the development of the ECM system integrated with surrounding VSMC are needed for higher vertebrates to function correctly.[21] Fibrillin-1 is not essential in the stabilisation of the elastic unit but instead in the assembly of the microfibril. Up-regulation of activin A works in conjunction with Fibrillin-1 and TGF-β signalling molecules to produce a fibroproliferative response.[21] CYR61 induction also functions to support cell adhesion and regulate matrix remodelling and is fundamental in the formation of large vessels and their integrity.[21]
Common variants in FBN1 can have effects on the gene and human phenotypes as well. For example, a common variant in Peruvian populations (E1297G) can cause a 2.2 cm reduction in height.[24]
Marfan syndrome
[edit]Marfan syndrome (MFS) is an autosomal dominant disorder that affects the connective tissues of bodily systems such as the eyes, cardiovascular system, skeletal system, skin, pulmonary system and the dura. MFS affects approximately 1 in 5,000 individuals.[25] MFS is not an easily diagnosed pathology with a scoring system called the Ghent nosology table used, rather than a single molecule test.[18] To diagnose MFS individuals that have no previous family history, two criteria must be met. Firstly, two different major organ systems must be affected, and secondly, a third organ system must be involved.[26]
MFS has a large hereditary component, with 80% of cases being inherited.[9] The remaining 20% of MFS cases occur from de novo mutations (new germline mutations not inherited from either parent) and results in the individual phenotypically displaying long and thin limbs and extremities, a curved spine usually resulting in thoracic scoliosis, hyperflexible joints, pectus excavatum (sunken chest), and retinal detachment.[25] De Novo mutations resulting in severe MFS have high expected mortality rates for neonates.[18] Classical MFS symptoms usually become noticeable during puberty or later in life; rarely does it develop in the earlier stages of life.[18] The most common skin manifestation of MFS is striae distensae where bands of skin are coloured red, purple and then white.[19] The skin epidermis is thin and flattened, and the upper protective skin layer is decreased in thickness.[19] This manifestation is characterised histologically by straight, thin collagen bundles arranged in a parallel to the skin and the elastic fibres.[19] Elastic fibres are denser in the upper dermis, and beneath this zone there is a localised absence of the elastic fibres. Between the borders of the striae and skin, there are curled, broken, reticular elastic fibres sometimes present.[21] These symptoms are responsible for cobweblike skin appearances in patients with MFS.[21]
Management of MFS covers many aspects, and includes lifestyle advice, physiotherapy, medication and surgery. [18] Management of MFS includes counselling on lifestyle to reduce and restrict physical activity, endo prophylaxis, serial imaging the aorta, β-blocker medication for aortic protection and prophylactic replacement of the aortic root.[18] In MFS affected adults, it is recommended they reduce emotional and physical stress and switch from high impact sports such as martial arts, football, basketball etc to isotonic, low impact exercise such as swimming, biking or jogging where the pulse rate lies approximately at <110 beats per minute.[18] Children should also follow similar guidelines to ensure correct management of MFS.[18]
MFS is caused by a mutation in the FBN1 gene positioned at chromosome 15q21.1 resulting in a deconstructed form of Fibrillin-1.[5] Fibrillin-1 is a 350-kDa, 2871-amino acid cystine-rich glycoprotein that is responsible for the amalgamation of elastin into the elastic fibres of the connective tissue in the extracellular matrix (ECM).[27][28] The fragility of the connective tissue usually results in aortic aneurysms due to the wall having the inability to withstand intraluminal pressure.[29] Defects in fibrillin-1 results in elevated TGF-β levels that directly correlate to MFS.[29]
Role of TGF-β
[edit]Transforming growth factor beta (TGF-β) is a paracrine regulatory protein responsible for embryonic processing, cell growth, apoptosis induction, and enhances collagen production and ECM remodelling.[29] In a non-MFS affected individual, the TGF-β protein is secreted from the cell to stimulate PAI-1 production and Smad2 phosphorylation.[21] The TGF-β protein binds with latency associated protein (LAP) at the N-terminal properties and one of three latent TGF-β binding proteins (LTBP1, 3 or 4) to form a small latent complex (SLC).[30] SLC then binds extracellularly to latent TGF-β binding protein (LTBP) forming a large latent complex (LLC), which includes an active cytokine.[16] The LLC attaches to the microfibrils of Fibrillin-1 via LTBP, allowing the preservation of inactive TGF-β [6]. TGF-β can only be activated through a series of regulated mechanisms; maintaining correct functioning in embryonic development.[29] Mutations in Fibrillin-1 cause elevated levels of TGF-β in the EC space due to LLC being unable to attach to the microfibrils and latent forms not being produced.[30] TGF-β forms a complex with its dimer receptors, to initiate a phosphorylation cascade.[31] This phosphorylation can cause failures such as an aortic aneurysm and prolapsed valves.[25]
Clinical symptoms of MFS such as aortic root dilation, pulmonary emphysema, atrioventricular valve changes and skeletal muscle myopathy are induced by altered TGF-β activation and signalling.[16] Aortic specific symptoms are closely related to excessive TGF-β signalling in the aortic root wall.[16] TGF-β antagonism via systemic administration of TGF-β neutralising antibody (NAb) averted the development of aortic pathologies associated with MDS, more specifically changes in the aortic wall and progressive aortic dilation.[16] Antagonism of TGF-β also further reduced MFS symptoms where it helped muscle regeneration, architecture and strength, pulmonary alveolar septation and mitral valve morphology.[16]
LLC that fails to be removed from the ECM is more vulnerable to be activated in a protease-dependent or independent manner.[16] MMP2 and MMP9 are select TGF-β activators and ligands and are found in higher levels in the tissues of patients affected with MFS. TGF-β in its complex and free-form can leach into the circulation due to the mutated ECM sequestration and increased LLC activation.[16]
Losartan
[edit]Losartan is an angiotensin II type 1 (AT1) receptor blocker known to antagonise TGF-β signalling via inhibiting the expression and activation of TGF-β.[16] Losartan can work independently or with β-blocker therapy to reduce rate of change in the aortic root diameter of MFS pathology.[16]
See also
[edit]Notes
[edit]
The 2018 version of this article was updated by an external expert under a dual publication model. The corresponding academic peer reviewed article was published in Gene and can be cited as: Lynn Y Sakai, Douglas R Keene, Marjolijn Renard, Julie De Backer (17 July 2016). "FBN1: The disease-causing gene for Marfan syndrome and other genetic disorders". Gene. Gene Wiki Review Series. 591 (1): 279–291. doi:10.1016/J.GENE.2016.07.033. ISSN 0378-1119. PMC 6639799. PMID 27437668. Wikidata Q38903109. |
References
[edit]- ^ a b c GRCh38: Ensembl release 89: ENSG00000166147 – Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000027204 – Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ a b Biery NJ, Eldadah ZA, Moore CS, Stetten G, Spencer F, Dietz HC (February 1999). "Revised genomic organization of FBN1 and significance for regulated gene expression". Genomics. 56 (1): 70–7. doi:10.1006/geno.1998.5697. PMID 10036187.
- ^ Faivre L, Gorlin RJ, Wirtz MK, Godfrey M, Dagoneau N, Samples JR, et al. (January 2003). "In frame fibrillin-1 gene deletion in autosomal dominant Weill-Marchesani syndrome". Journal of Medical Genetics. 40 (1): 34–6. doi:10.1136/jmg.40.1.34. PMC 1735272. PMID 12525539.
- ^ Romere C, Duerrschmid C, Bournat J, Constable P, Jain M, Xia F, et al. (April 2016). "Asprosin, a Fasting-Induced Glucogenic Protein Hormone". Cell. 165 (3): 566–79. doi:10.1016/j.cell.2016.02.063. PMC 4852710. PMID 27087445.
- ^ Jacquinet A, Verloes A, Callewaert B, Coremans C, Coucke P, de Paepe A, et al. (April 2014). "Neonatal progeroid variant of Marfan syndrome with congenital lipodystrophy results from mutations at the 3' end of FBN1 gene". European Journal of Medical Genetics. 57 (5): 230–4. doi:10.1016/j.ejmg.2014.02.012. PMID 24613577.
- ^ a b Ramachandra CJ, Mehta A, Guo KW, Wong P, Tan JL, Shim W (2015). "Molecular pathogenesis of Marfan syndrome". International Journal of Cardiology. 187: 585–91. doi:10.1016/j.ijcard.2015.03.423. PMID 25863307.
- ^ Quondamatteo F, Reinhardt DP, Charbonneau NL, Pophal G, Sakai LY, Herken R (December 2002). "Fibrillin-1 and fibrillin-2 in human embryonic and early fetal development". Matrix Biology. 21 (8): 637–46. doi:10.1016/s0945-053x(02)00100-2. PMID 12524050.
- ^ a b Votteler M, Berrio DA, Horke A, Sabatier L, Reinhardt DP, Nsair A, et al. (June 2013). "Elastogenesis at the onset of human cardiac valve development". Development. 140 (11): 2345–53. doi:10.1242/dev.093500. PMC 3912871. PMID 23637335.
- ^ Ammash NM, Sundt TM, Connolly HM (January 2008). "Marfan syndrome-diagnosis and management". Current Problems in Cardiology. 33 (1): 7–39. doi:10.1016/j.cpcardiol.2007.10.001. PMID 18155514.
- ^ "FBN1 fibrillin 1". Entrez Gene.
- ^ Online Mendelian Inheritance in Man (OMIM): FIBRILLIN 1; FBN1 - 134797
- ^ Buchan JG, Alvarado DM, Haller GE, Cruchaga C, Harms MB, Zhang T, et al. (October 2014). "Rare variants in FBN1 and FBN2 are associated with severe adolescent idiopathic scoliosis". Human Molecular Genetics. 23 (19): 5271–82. doi:10.1093/hmg/ddu224. PMC 4159151. PMID 24833718.
- ^ a b c d e f g h i j k l m Matt P, Schoenhoff F, Habashi J, Holm T, Van Erp C, Loch D, et al. (August 2009). "Circulating transforming growth factor-beta in Marfan syndrome". Circulation. 120 (6): 526–32. doi:10.1161/CIRCULATIONAHA.108.841981. PMC 2779568. PMID 19635970.
- ^ a b c d e f Katz KW, Greathead MM, Cook RC, Britz R (June 1976). "Experiences in the diagnosis of brucellosis in dairy cows". Journal of the South African Veterinary Association. 47 (2): 97–100. PMID 940103.
- ^ a b c d e f g h i von Kodolitsch Y, Robinson PN (June 2007). "Marfan syndrome: an update of genetics, medical and surgical management". Heart. 93 (6): 755–60. doi:10.1136/hrt.2006.098798. PMC 1955191. PMID 17502658.
- ^ a b c d Bergman R, Nevet MJ, Gescheidt-Shoshany H, Pimienta AL, Reinstein E (August 2014). "Atrophic skin patches with abnormal elastic fibers as a presenting sign of the MASS phenotype associated with mutation in the fibrillin 1 gene". JAMA Dermatology. 150 (8): 885–9. doi:10.1001/jamadermatol.2013.10036. PMID 24740214.
- ^ Keene DR, Jordan CD, Reinhardt DP, Ridgway CC, Ono RN, Corson GM, et al. (August 1997). "Fibrillin-1 in human cartilage: developmental expression and formation of special banded fibers". The Journal of Histochemistry and Cytochemistry. 45 (8): 1069–82. doi:10.1177/002215549704500805. PMID 9267468.
- ^ a b c d e f g h i j k l m n Martínez-Quintana E, Rodríguez-González F, Garay-Sánchez P, Tugores A (August 2014). "A novel fibrillin 1 gene mutation leading to marfan syndrome with minimal cardiac features". Molecular Syndromology. 5 (5): 236–40. doi:10.1159/000358846. PMC 4188161. PMID 25337071.
- ^ Charbonneau NL, Carlson EJ, Tufa S, Sengle G, Manalo EC, Carlberg VM, et al. (August 2010). "In vivo studies of mutant fibrillin-1 microfibrils". The Journal of Biological Chemistry. 285 (32): 24943–55. doi:10.1074/jbc.M110.130021. PMC 2915730. PMID 20529844.
- ^ a b c Barrett PM, Topol EJ (January 2013). "The fibrillin-1 gene: unlocking new therapeutic pathways in cardiovascular disease". Heart. 99 (2): 83–90. doi:10.1136/heartjnl-2012-301840. PMID 22942299. S2CID 19962009.
- ^ Asgari S, Luo Y, Akbari A, Belbin GM, Li X, Harris DN, et al. (June 2020). "A positively selected FBN1 missense variant reduces height in Peruvian individuals". Nature. 582 (7811): 234–239. Bibcode:2020Natur.582..234A. doi:10.1038/s41586-020-2302-0. PMC 7410362. PMID 32499652.
- ^ a b c Summers KM, Nataatmadja M, Xu D, West MJ, McGill JJ, Whight C, et al. (November 2005). "Histopathology and fibrillin-1 distribution in severe early onset Marfan syndrome". American Journal of Medical Genetics. Part A. 139 (1): 2–8. doi:10.1002/ajmg.a.30981. PMID 16222666. S2CID 33663469.
- ^ Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, Devereux RB, et al. (July 2010). "The revised Ghent nosology for the Marfan syndrome". Journal of Medical Genetics. 47 (7): 476–85. doi:10.1136/jmg.2009.072785. hdl:1854/LU-1013955. PMID 20591885. S2CID 13895128.
- ^ Sakai LY, Keene DR, Engvall E (December 1986). "Fibrillin, a new 350-kD glycoprotein, is a component of extracellular microfibrils". The Journal of Cell Biology. 103 (6 Pt 1): 2499–509. doi:10.1083/jcb.103.6.2499. PMC 2114568. PMID 3536967.
- ^ Smallridge RS, Whiteman P, Werner JM, Campbell ID, Handford PA, Downing AK (April 2003). "Solution structure and dynamics of a calcium binding epidermal growth factor-like domain pair from the neonatal region of human fibrillin-1". The Journal of Biological Chemistry. 278 (14): 12199–206. doi:10.1074/jbc.M208266200. PMID 12511552.
- ^ a b c d Benke K, Ágg B, Szilveszter B, Tarr F, Nagy ZB, Pólos M, et al. (2013). "The role of transforming growth factor-beta in Marfan syndrome". Cardiology Journal. 20 (3): 227–34. doi:10.5603/CJ.2013.0066. PMID 23788295.
- ^ a b Dietz HC (October 2007). "2006 Curt Stern Award Address. Marfan syndrome: from molecules to medicines". American Journal of Human Genetics. 81 (4): 662–7. doi:10.1086/521409. PMC 2227916. PMID 20529617.
- ^ Chaudhry SS, Cain SA, Morgan A, Dallas SL, Shuttleworth CA, Kielty CM (January 2007). "Fibrillin-1 regulates the bioavailability of TGFbeta1". The Journal of Cell Biology. 176 (3): 355–67. doi:10.1083/jcb.200608167. PMC 2063961. PMID 17242066.
Further reading
[edit]- Hayward C, Brock DJ (1998). "Fibrillin-1 mutations in Marfan syndrome and other type-1 fibrillinopathies". Human Mutation. 10 (6): 415–23. doi:10.1002/(SICI)1098-1004(1997)10:6<415::AID-HUMU1>3.0.CO;2-C. PMID 9401003. S2CID 41867728.
- Robinson PN, Godfrey M (January 2000). "The molecular genetics of Marfan syndrome and related microfibrillopathies". Journal of Medical Genetics. 37 (1): 9–25. doi:10.1136/jmg.37.1.9. PMC 1734449. PMID 10633129.
- Handford PA (December 2000). "Fibrillin-1, a calcium binding protein of extracellular matrix". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 1498 (2–3): 84–90. doi:10.1016/s0167-4889(00)00085-9. PMID 11108952.
- Robinson PN, Booms P, Katzke S, Ladewig M, Neumann L, Palz M, et al. (September 2002). "Mutations of FBN1 and genotype-phenotype correlations in Marfan syndrome and related fibrillinopathies". Human Mutation. 20 (3): 153–61. doi:10.1002/humu.10113. PMID 12203987. S2CID 19479210.
- Adès LC, Holman KJ, Brett MS, Edwards MJ, Bennetts B (April 2004). "Ectopia lentis phenotypes and the FBN1 gene". American Journal of Medical Genetics. Part A. 126A (3): 284–9. doi:10.1002/ajmg.a.20605. PMID 15054843. S2CID 19069429.
- Milewicz DM, Dietz HC, Miller DC (March 2005). "Treatment of aortic disease in patients with Marfan syndrome". Circulation. 111 (11): e150-7. doi:10.1161/01.CIR.0000155243.70456.F4. PMID 15781745.
- Boileau C, Jondeau G, Mizuguchi T, Matsumoto N (May 2005). "Molecular genetics of Marfan syndrome". Current Opinion in Cardiology. 20 (3): 194–200. doi:10.1097/01.hco.0000162398.21972.cd. PMID 15861007. S2CID 26269805.
- Whiteman P, Hutchinson S, Handford PA (2006). "Fibrillin-1 misfolding and disease". Antioxidants & Redox Signaling. 8 (3–4): 338–46. doi:10.1089/ars.2006.8.338. PMID 16677079.
External links
[edit]- GeneReviews/NCBI/NIH/UW entry on Marfan Syndrome
- Overview of all the structural information available in the PDB for UniProt: P35555 (Fibrillin-1) at the PDBe-KB.